 This winter has appeared to come and go with little more than a whimper and if you’re like me you’re probably itching to get outside and enjoy the fantastic weather that is around the corner. For some individuals this will entail running, biking and recreational sports. The one unifying factor for all of these people is that a significant percentage will experience knee pain that will either affect their performance or prevent them from participating all together. Although there are a number of different possible causes for knee pain in active individuals, patellofemoral pain syndrome (PFPS) is one of the most prevalent and accounts for 25-40% of all knee pain complaints seen in sports injury clinics. The purpose of this article will be to shed light on the cause, prevention strategies and therapies of PFPS.
This winter has appeared to come and go with little more than a whimper and if you’re like me you’re probably itching to get outside and enjoy the fantastic weather that is around the corner. For some individuals this will entail running, biking and recreational sports. The one unifying factor for all of these people is that a significant percentage will experience knee pain that will either affect their performance or prevent them from participating all together. Although there are a number of different possible causes for knee pain in active individuals, patellofemoral pain syndrome (PFPS) is one of the most prevalent and accounts for 25-40% of all knee pain complaints seen in sports injury clinics. The purpose of this article will be to shed light on the cause, prevention strategies and therapies of PFPS.
What is Patellofemoral Pain Syndrome (PFPS)?
Patellofemoral Pain Syndrome (PFPS) is defined as diffuse pain over the front of the knee that is aggravated by movements that increase the compressive force of the knee (patellofemoral) joint. These activities include squatting, going up and down stairs, prolonged sitting and running. PFPS has been described as an orthopaedic enigma, in that an alarmingly high number of individuals with PFPS have recurrent or chronic pain.
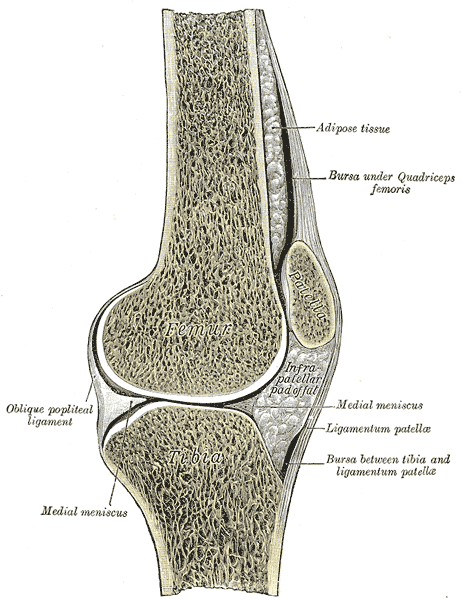
Patellofemoral Pain Syndrome Pain generating Structures
There is limited evidence to suggest that a number of local structures contribute to pain in individuals with PFPS. These structures include the infrapatellar fat pad, increased water content in subchondral patellar and bone marrow lesions. There is no new evidence that the lateral retinaculum contributes to pain in individuals with PFP. There are some theories that suggest the distal attachment sites of the IT band are pain generating structures. These include the attachment site to gerdy’s tubercle on the (anterior-lateral) tibia and the fibular head. There is no new evidence to support these claims.
Is Patellofemoral Pain Syndrome a self limiting condition or should I be worried about future complications? (PFPs & PFOA)
A subject of major interest and debate is the possibility of a continuum from PFPS to arthritis (osteoarthritis) of the patellofemoral joint (PFOA). Although it is possible that there is a subgroup of PFPS that goes on to develop PFOA, there is no evidence as of yet support this view.
Quadriceps Activation and Patellofemoral Pain Syndrome
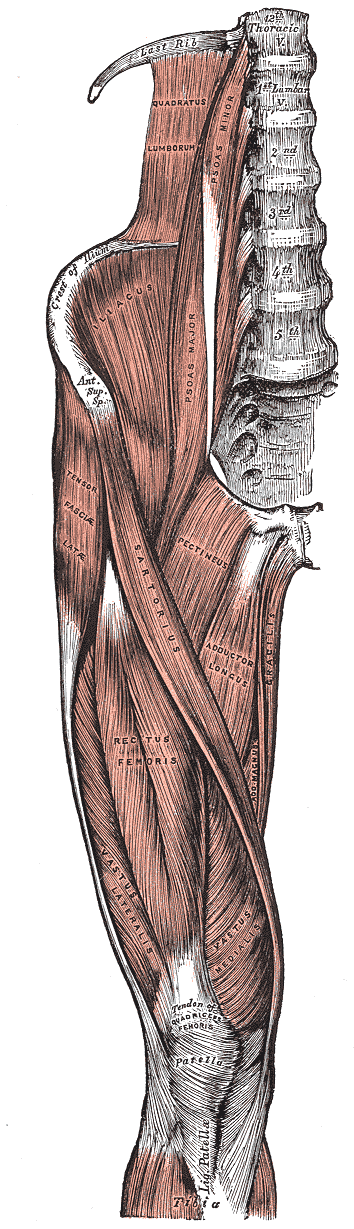
One of the proposed mechanisms of PFPS is that there is an imbalance between the muscular pull of the lateral part of the quadriceps (vastus lateralis) muscle compared to the medial (VMO). Proponents of this theory believe this causes a tracking issue with the patella leading to PFPS. However, functional MRI, used to display activation of the quadriceps has raised doubts that altered quadriceps activation patterns are seen in individuals with PFPS.
Foot Mechanism and Patellofemoral Pain Syndrome

The relationship between the biomechanics of the foot and PFPS remains unclear. Studies have shown that individuals with PFPS demonstrate increased rear-foot eversion – pronation in the picture. Calcaneal eversion may be linked with increased hip adduction. Rear-foot eversion is when your heel (calcaneus) bends towards the outside of your leg. This causes the arches (medial) of your feet to flatten, your shins (tibia) to rotate inwards (internal) and your knees to approximate (valgus loading). Nevertheless, no studies have yet to identify altered foot biomechanics as a predictor of PFPS.
Knee structure and biomechanics in relation to Patellofemoral Pain Syndrome
New evidence suggests that abnormal structure or alignment of the knee cap and femur (PFJ) may lead to cartilage damage and focal areas of loading and stress that manifests as bone marrow lesions (BMLs). The relationship between structure and biomechanics is not known. It is possible that structural abnormalities coupled with poor biomechanics will increase the likelihood of PFPS. On the other hand if there is normal structure then the biomechanics may not matter.
Taping and Patellofemoral Pain Syndrome
A review of 21 studies found that tailored patellar taping (customized to control for lateral tilt, glide and spin) provides immediate pain relief and promoted an earlier activation of vastus medialis oblique (VMO) contraction. Untailored patellar taping also demonstrated immediate pain relief; however, the results were not as prominent as the tailored group. Therefore, there might be promise for therapies such as kin taping.
Patellofemoral Pain Syndrome and gluteus medius activation
The gluteus medius is an important abductor and stabilizer of the hip during a single leg stance. Evidence has shown that gluteus medius activation is delayed and of shorter duration in patients with PFPS. Studies have also shown excessive hip adduction and/or internal rotation in women with PFPS. It should be noted that the glut med is not strong enough to support the hip and that the opposite (contralateral) psoas major is important for stabilizing the low back and preventing hip drop.
Treatment options for Patellofemoral Pain Syndrome
- Facilitation (Neurological activation) and improved muscular endurance of the gluteus medius.
- Previous Studies have demonstrated a 75% improvement in symptoms individuals with PFPS who perform rehabilitation exercises for the gluteus medius.
- Facilitation of the glut med includes electrical stimulation with exercise, acupuncture with electricity and rehabilitative exercises, such as: side lying leg abduction with a resistance band, hip hikes and clam exercises.
- Tailored Kin Taping of the knee joint to control undesired movement of the patella.
- Minimize rear-foot eversion by working on short foot exercises or using orthotics.
*All of the information provided is based on the current evidence from the 3rd International patellofemoral pain symposium*
If you have any questions regarding any of the information provided, please visit sportsrehabandwellness.ca.

